BAME COVID-19 DEATHS – What do we know? Rapid Data & Evidence Review
May 5, 2020
Abdul Razaq1, Dominic Harrison2, Sakthi Karunanithi3, Ben Barr4, Miqdad Asaria5, Ash Routen6, Kamlesh Khunti7
1. Consultant in Public Health, Lancashire County Council, Visiting Senior Fellow, University of Suffolk
2. Director of Public Health, Blackburn with Darwen Council, Visiting Professor University of Central Lancashire (UCLAN)
3. Director of Public Health, Lancashire County Council
4. Professor in Applied Public Health Research, University of Liverpool
5. Assistant Professorial Research Fellow, London School of Economics
6. Research Associate, University of Leicester
7. Professor in Primary Care Diabetes & Vascular Medicine, University of Leicester
On behalf of the Oxford COVID-19 Evidence Service Team
Centre for Evidence-Based Medicine, Nuffield Department of Primary Care Health Sciences
University of Oxford
Editorial input from Professor Trisha Greenhalgh
Correspondence to Abdul.Razaq@lancashire.gov.uk
PDF to Download
VERDICT
Evidence indicates markedly higher mortality risk from COVID-19 among Black, Asian and Minority Ethnic (BAME) groups, but deaths are not consistent across BAME groups. Similarly, adverse outcomes are seen for BAME patients in intensive care units and amongst medical staff and Health and Care Workers. The exact reasons for this increased risk and vulnerability from COVID-19 in BAME populations are not known. There may be a number of contributing factors in the general population such as overrepresentation of BAME populations in lower socio-economic groups, multi-family and multi-generational households, co-morbidity exposure risks, and disproportionate employment in lower band key worker roles. For Health and Care workers, there are increased health and care setting exposure risks.
BACKGROUND
The UK has a large and diverse Black, Asian and Minority Ethnic community (BAME), which account for around 14% of the population in England and Wales. Worryingly there is early evidence of an association between ethnicity and COVID-19 incidence and adverse health outcomes. For example, observational data from the Intensive Care National Audit and Research Centre, show a third of COVID-19 patients admitted to critical care units are from BAME groups. There are also concerns that healthcare and other key workers who belong to BAME groups are particularly at risk.
With data on COVID-19 in BAME populations emerging daily, this rapid review aimed to evaluate the evidence on plausible associations between ethnicity and COVID-19 incidence and adverse health outcomes in the general population and people working in health and social care.
METHOD
An ongoing Google Scholar literature search has been conducted since the COVID-19 outbreak began, and this has been updated through publications on MedRxiv preprint and social media.
EMERGING EVIDENCE
BAME Deaths by Ethnicity in England
Analysis of hospital death data in England by the Institute for Fiscal Studies (IFS) show deaths per capita are not consistent across BAME groups, and they are markedly greater in Black Carribean and Black Other groups compared to all other ethnicities (except ‘Other ethnic group’). For example, per capita, Black Carribean deaths are over twice those of Bangladeshi and Pakistani populations. It is important to note that compared to the White British population per capita deaths are markedly greater in Indian, Other Black, Black Carribbean and Other Ethnic group (see the figure below, but note these data are not adjusted for potential explanatory factors such as age, geography, occupational exposure etc.).

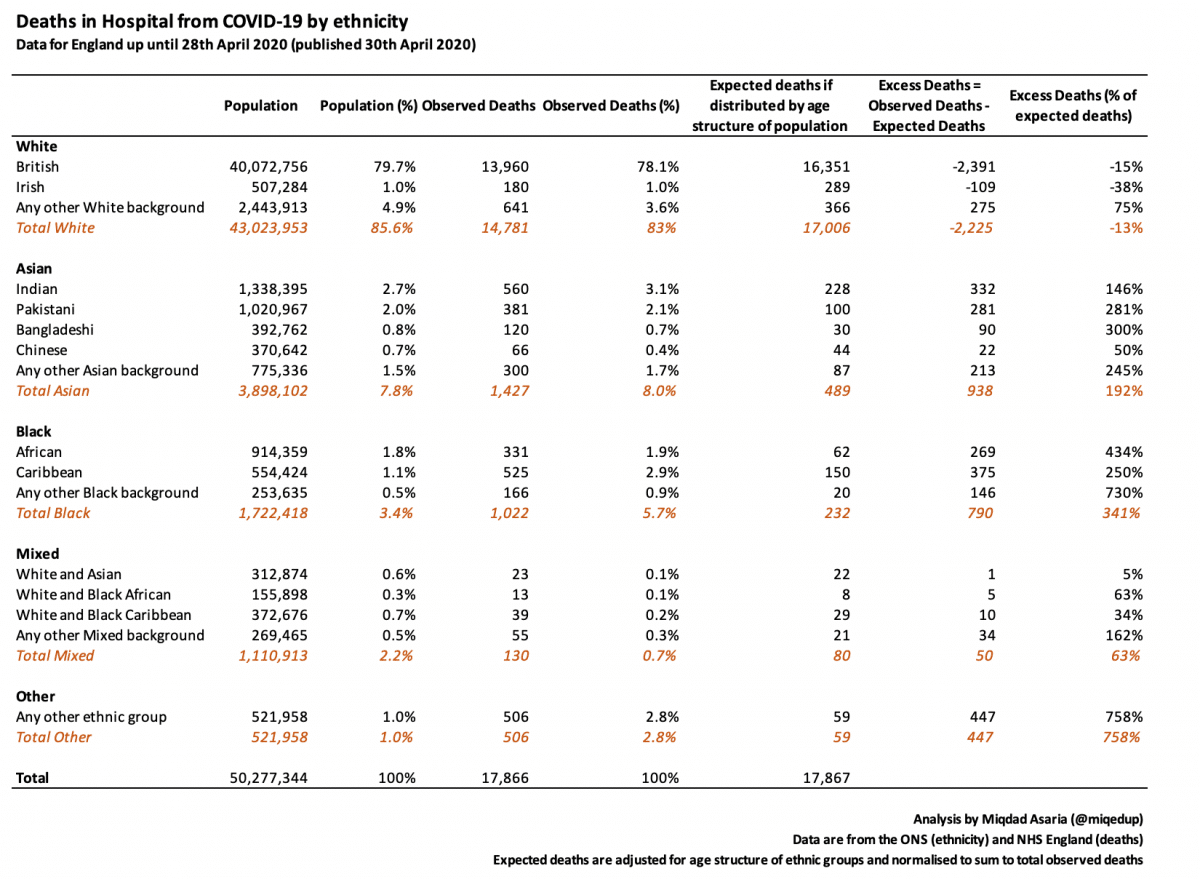
Analysis of NHS England hospital death data shows excess deaths vary by BAME group (See table below, final column on right). Excess deaths (observed vs. expected) are around 1.5 times higher than expected for the Indian population, 2.8 times higher for the Pakistani population, and 3 times higher in Bangladeshis. Excess deaths are 4.3 times higher for the Black African population, 2.5 times for the Black Caribbean population, and 7.3 times higher for Black Other Background individuals. Excess deaths are 1.6 times higher for the Mixed Any Other Background population.
Using NHS England and ONS data, Statista compared the number of COVID-19 deaths in BAME groups compared to their proportion of the country’s total population. This brief analysis shows there have been 801 deaths in the Black ethnic group as of April 17, accounting for 5.8% of COVID-19 deaths. Given this ethnic group accounts for 3.5% of the total population in England, the share of deaths in Black individuals is 66% higher than this groups proportion of the total population. The number of Asian deaths is similar to their share of the total population.
Further analysis of hospital death data in England and Wales by the IFS has attempted to adjust for the greater occurrence of COVID-19 cases in urban areas with high BAME density (e.g. London and Birmingham), and the majority of BAME groups being on average younger than White British populations. The IFS report details predicted number of hospital deaths by ethnic group if geography (region of residence) and demographic (age and sex) factors were the only relevant determinants of increased COVID-19 deaths in BAME groups.
By comparing the ratio of predicted deaths to actual hospital deaths, an estimate of excess death beyond those that can be explained by demographics and geography can be calculated. The ratio varies across BAME groups, from 1.8 for Black Caribbeans, to 2.9 for Pakistanis and 3.7 for Black Africans (See the difference between dark green and yellow bars in the figure below. Note data in the graph are presented relative to White British populations).

BAME Patient Characteristics and Patient Outcome in Intensive Care Units (ICU)
The first indication of an association between BAME and COVID-19 came from data presented by the Intensive Care National Audit and Research Centre (ICNARC), which focused on patients critically ill with confirmed COVID-19 reported to ICNARC up to 23 April 2020.
Concerning BAME patient characteristics, these data show that 34% of BAME patients with confirmed COVID-19 are admitted to ICU as compared to 12% for viral pneumonia. There is a clear social gradient for patients with confirmed COVID-19 admitted to ICU, with the most deprived nearly twice as likely than the least deprived by Index of Multiple Deprivation (IMD) quintile.
On outcomes, approximately half of BAME patients with COVID-19 were discharged alive from ICU. Asian patients with COVID-19 were 3 times more likely to die in ICU than patients with viral pneumonia. Mixed ethnicity patients with COVID-19 were 2 times more likely to die in ICU than patients with viral pneumonia. Black ethnicity patients with COVID-19 were 4 times more likely to die in ICU than patients with viral pneumonia. Other ethnicity patients with COVID-19 were 2.5 times more likely to die in ICU than patients with viral pneumonia.
Forty percent of Asian, Black and Other BAME patients required renal support in ICU, and there is a clear social gradient with those in IMD quintile 5 (most deprived) nearly twice as likely to require renal support as IMD quintile 1 (least deprived).
The pattern of ICU outcomes by ethnic group broadly reflect the pattern of overall COVID-19 mortality by ethnic groups, suggesting that ICU deaths follow the overall death risk pattern for BAME communities.
BAME Health and Care Worker Deaths
Data published in the Health Service Journal detail the disproportionately high rate of BAME individuals among Health and Care Workers who have died from COVID-19. Among all staff employed by the NHS, BAME groups account for approximately 21%, including roughly 20% among nursing and support staff and 44% among medical staff (i.e doctors and dentists). Initial analysis of health and care worker BAME COVID-19 deaths suggest they account for 63%, 64% and 95% of overall deaths in the aforementioned staff groups respectively.
International Evidence
In the United States the latest available COVID-19 mortality rate for Black Americans is 2.4 times higher than the rate for Latino populations, 2.5 times higher than Asian individuals, and 2.7 times higher than White populations. For every 100,000 Americans (of their respective groups), around 26 Black individuals have died, along with 11 Latino, 10 Asian and 9 White.
CONCLUSIONS
There is early observational evidence to suggest that COVID-19 hospital deaths among the general population in England are greater in BAME groups compared to White British groups. In addition the number of deaths is not consistent across BAME groups, with per capita deaths and excess deaths highest among Black populations. There is also international evidence from the US to show non-uniform COVID-19 deaths across BAME groups.
Data on Health and Care Worker deaths show disproportionately high deaths in BAME populations, with the greatest number occurring in medical staff when compared to other staff categories.
Exact reasons for this increased risk in BAME populations are not known. There may be a number of factors that increase BAME COVID-19 risks and vulnerability in the general population, such as overrepresentation of BAME populations in lower socio-economic groups; multi-family and multi-generational households leading to increased risk of transmission due to the lockdown; co-morbidity exposure risks especially for CVD, diabetes, renal conditions and complex multi-morbidities in ICU; and there is disproportionate BAME employment in lower band key worker roles who either work in high exposure care environments or are unable to implement safe social distancing due to their roles. In addition, for Health and Care Workers, there are increased health and care setting COVID-19 exposure risks.
Disclaimer: the article has not been peer-reviewed; it should not replace individual clinical judgement and the sources cited should be checked. The views expressed in this commentary represent the views of the authors and not necessarily those of the host institution, the NHS, the NIHR, or the Department of Health and Social Care. The views are not a substitute for professional medical advice.
AUTHORS
AR has formerly held positions as Director of Public Health for fifteen years and has extensive senior executive Public Health experience in the NHS and local government in the UK. He is currently Consultant in Public Health at Lancashire County Council and Visiting Senior Fellow, University of Suffolk. He is a member of the UK Faculty of Public Health Special Interest Group on Pakistan and is a Fellow of the UK Faculty of Public Health. KK is Director of Leicester Diabetes Centre and Director of The Centre for Black and Minority Ethnic Health (NIHR Applied Research Collaboration East Midlands) at the University of Leicester.
REFERENCES
All sources of evidence used in this review are available via the hyperlinks above.

