Probable healthcare associated infections in England
October 9, 2020
Daniel Howdon, Jason Oke, Tom Jefferson, Carl Heneghan
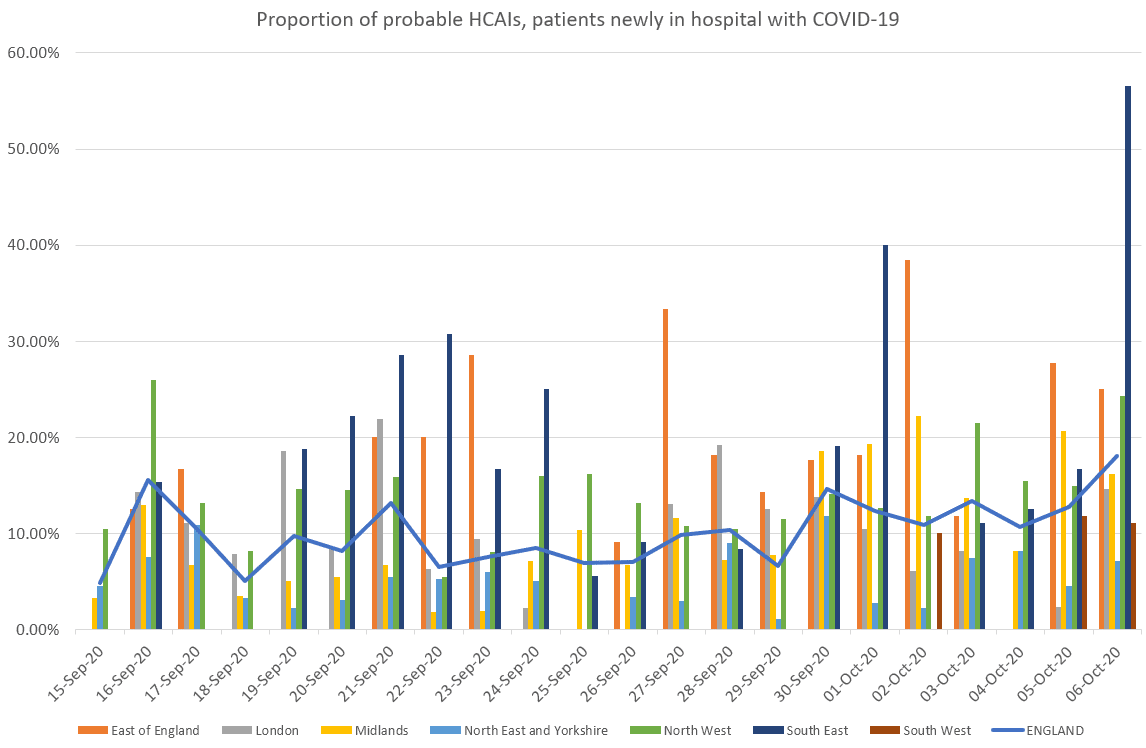
Recent days have seen an apparent rise in the proportion of patients newly admitted in hospital with COVID-19 that represent probable healthcare-associated infections (HCAIs), with these comprising 18% of all new hospital cases on 6 October. This is most apparent in the North West of England, where HCAIs made up 24% of all patients on this date.
NHS England produces a daily update on new hospitalisations by region. As of 22 September, the daily information from situation reports on the number of hospital admissions and diagnoses for COVID-19 were made available. This contains several data series which categorise patients based on whether they tested positive for COVID-19 before admission, whether they were admitted from a care home and, if applicable, the point in their hospital stay at which they were diagnosed with COVID-19.
We used these data to construct a measure of the number of patients in hospital who are test-positive for COVID-19. We consider patients to be newly in hospital with COVID-19 at the point of admission (if they tested positive prior to admission) or at the point at which they test positive (if they test positive in hospital). In line with NHS England guidance, we consider patients who test positive after over 7 days in hospital to be probable healthcare-associated infections (HCAIs).
Update 15th October:
Up to 17.3% (111/640) admissions are probable nosocomials on the 12th October.
Estimated new hospital cases minus the estimated new admissions to hospital from the community and the percentages by area:
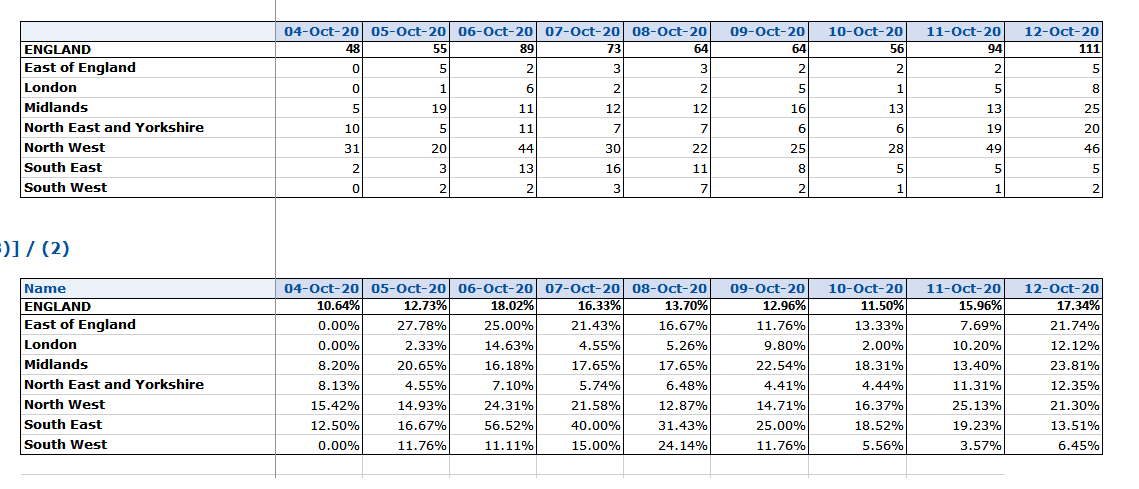
9th October
 In the NHS England data for the 6th October, there are several different measures reported (see the definitions here).
In the NHS England data for the 6th October, there are several different measures reported (see the definitions here).
- The number of estimated daily admissions and new diagnoses for COVID-19 (n=524 on most recent reporting date).
- Estimated new hospital cases (n=494): excludes anybody who had previously had a COVID-19 admission.
- Estimated new admissions to hospital from the community (n=405): excludes those who test positive more than 7 days after admission and swab.
Using these data we can then estimate the probable number of HCAIs as 89 (18%) based on the number of new cases (n=494 on the most recent reporting date) minus the estimated new admissions to hospital from the community (n=405). Thirty people were (for unspecified reasons) readmitted with COVID-19 (number 1 from the list minus number 2).
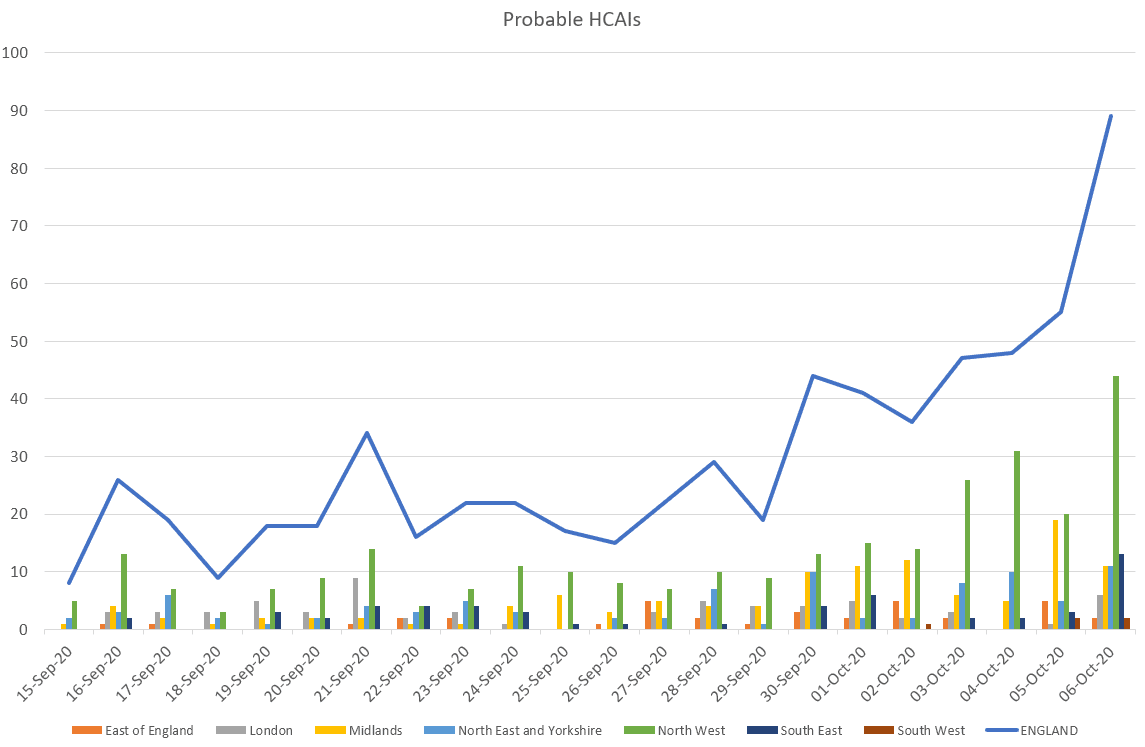
Using this approach we used data from 15 September, the first day in recent months on which there were over 150 admissions. While only three days since 15 September had seen these cases form over 10% of the total of new patients in hospital with COVID-19, each of the last seven days reported has seen probable HCAIs from over 10% of newly reported hospitalised patients.
The most recent date of reporting (6 October) shows a record high, with over 18% of hospitalisations being patients diagnosed after over 7 days in hospital. This appears to be particularly notable in the North West, where 17% (163/967) in the last week and 24% (44/181) on 6 October of those patients newly in hospital with COVID-19 were probable HCAIs.
Improving the quality and granularity of the data is vital for performing in-depth analysis of the issues. Providing data at the trust level would permit a more thorough understanding of the HCAI problem.
Daniel Howdon is a Senior Research Fellow in Health Economics, Leeds Institute of Health Sciences. Bio here
Carl Heneghan is Professor of Evidence-Based Medicine, Director of the Centre for Evidence-Based Medicine and Director of Studies for the Evidence-Based Health Care Programme. (Full bio and disclosure statement here)
Jason Oke is a Senior Statistician at the Nuffield Department of Primary Care Health Sciences and Module Coordinator for Statistical Computing with R and Stata (EBHC Med Stats), and Introduction to Statistics for Health Care Research (EBHC), as part of the Evidence-Based Health Care Programme.
Tom Jefferson is an Epidemiologist. Disclosure statement is here
Disclaimer: the article has not been peer-reviewed; it should not replace individual clinical judgement, and the sources cited should be checked. The views expressed in this commentary represent the views of the authors and not necessarily those of the host institution, the NHS, the NIHR, or the Department of Health and Social Care. The views are not a substitute for professional medical advice.

