What is the effectiveness of protective gowns and aprons against COVID-19 in primary care settings?
April 16, 2020
Briana Coles, University of Leicester
Chris Burton, University of Sheffield
Kamlesh Khunti, University of Leicester
Trisha Greenhalgh and Xin Hui Chan, University of Oxford
Lawrence Ross, Children’s Hospital, Los Angeles
Series editor:
Trish Greenhalgh
On behalf of the Oxford COVID-19 Evidence Service Team
Centre for Evidence-Based Medicine
Nuffield Department of Primary Care Health Sciences
University of Oxford
Correspondence to kk22@leicester.ac.uk
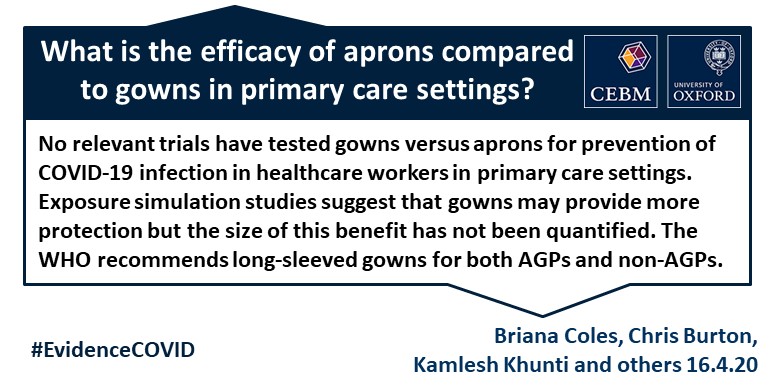
VERDICT
This review found no relevant trials comparing the effectiveness of gowns against aprons. Exposure simulation studies suggest that the risk of exposure in healthcare workers is greater with aprons than with gowns but do not provide sufficient data to quantify those risks in the context of primary or community care activity. The WHO recommends long-sleeved non-sterile gowns and gloves for both aerosol-generating procedures (AGPs) and non-AGPs. The US CDC has suggested using aprons over gowns as an additional measure to provide protection from contamination of garments during aerosol generating procedures.
Properly used protective clothing is only one component of a package of personal protective measures (which also includes gloves, mask, eye protection and hand washing / disinfection).
BACKGROUND
Healthcare workers (HCW) in primary care settings appear to be at greater risk of COVID-19 infection than the general population (1). The main transmission routes for COVID-19 are thought to be via droplet spread and fomites from hand to mucous membranes (2). Protective clothing serves to reduce spread of droplets or other body fluids to the HCW’s skin and clothing and hence reduce the risk of secondary spread to hands and then to mucous membranes. Recommendations for Aerosol Generating Procedures (AGPs) consistently recommend a full body gown, often with a waterproof apron on top. Some recommendations for lower intensity settings such as clinical consultation or examination in primary or community care (including NHS England guidelines published April 6, 2020), recommend an apron rather than gown as part of a bundle of protection with mask, gloves, and situation-specific eye protection (3). This recommendation for apron rather than gown has generated concern among primary care and community HCWs who are concerned their protection may be inadequate.
Policy guidance from various bodies (e.g. Public Health England, World Health Organization (WHO)) emphasizes the need to assess the contagion risk of an encounter and use the recommended combination of equipment for that situation.
The WHO distinguishes different levels of risk (4)– for example:
- Standard precautions e.g. for staff conducting triage: hand hygiene + require any patient with suspected COVID-19 to wear a facemask;
- ‘Contact and droplet precautions’ for suspected or confirmed case of COVID-19 not involving AGPs: requires hand hygiene, surgical mask, gown, goggles, gloves;
- ‘Airborne precautions’ for suspected or confirmed case of COVID-19 requiring healthcare facility admission and AGP: requires hand hygiene, respirator mask, gown, goggles, gloves;
- Collection of specimens for laboratory diagnosis: if undertaken via an AGP, requires hand hygiene, respirator mask, gown, goggles, gloves plus additional precautions
WHO guidance recommends gowns, not aprons, for both AGPs and non-AGPs in all circumstances except initial triage. For contact and droplet precautions, the recommendation is “a clean, non-sterile, long-sleeved gown” as well as gloves. For AGPs, the guidance states: “wear a clean, non-sterile, long-sleeved gown and gloves. If gowns are non fluid-resistant, HCWs should use a waterproof apron for procedures expected to create high volumes of fluid that may penetrate the gown.” (4)
In other words, there is no situation for which the WHO recommends a plastic apron of the kind supplied to primary care staff in the UK. US CDC Guidelines indicate that organisations experiencing profound shortages of gowns may use disposable aprons as a ‘last-resort’, recognising that they cannot be considered PPE.(5)
SEARCH STRATEGY
We performed a rapid search of PubMed and Medline databases without date restrictions to identify any relevant randomised trials, meta-analyses, or reviews. We used the following key words: “Coronavirus”, “COVID-19”, “Severe Acute Respiratory Syndrome”, “SARS”, “MERS”, “influenza”, “respiratory tract infections”, “gown”, “apron”, “smock”, “protective clothing” and the following Mesh term: Influenza, Human.
We identified two Cochrane systematic reviews that were directly relevant to our question (6, 7). Verbeek et al. reviewed personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. An update of the Verbeek review was published very recently (April 2020) and did not find any additional studies.(8) Jefferson et al. reviewed physical interventions to interrupt or reduce the spread of respiratory viruses. This was most recently published in 2011; an update is underway. We identified a third systematic review on transmission of respiratory syncytial virus (9) that found no evidence for a protective effect of gowns. We found no additional randomised controlled trials. Additional targeted searching did not find relevant exposure simulation studies other than two reported in Verbeek et al., which compared gowns with aprons (10, 11).
We used the GRADE domains of risk of bias, imprecision, inconsistency, indirectness, and publication bias to assess the usefulness of the evidence. Overall, we found the usefulness of evidence in the reviews to be low because of indirectness, imprecision and risk of bias.
- Indirectness: clinical studies were conducted in hospital settings (some involving exposure to AGPs) rather than in community / primary care settings; they involved non-COVID-19 illness although these were all respiratory illnesses with airborne spread. Exposure simulation studies used medium-heavy grade aprons (e.g. endoscopy apron) which are more substantial than the lightweight disposable aprons currently in widespread use in primary care settings.
- Imprecision: We found no head to head clinical studies comparing apron versus gown. Other studies were relatively small and crucially included clothing as part of a bundle of protective equipment making. None were able to demonstrate a specific effect of clothing after adjusting for other elements of protection.
- Risk of bias: clinical case control studies relied on retrospective self-report of protective clothing use, largely once HCWs case status was known.
Summary of findings from most useful papers
Randomised Controlled Trials
We found no randomised controlled trials, comparing protective clothing (specifically, gowns or aprons) with either another type of protective clothing or none, in which respiratory infection was an outcome.
Case Control and Cohort Studies
Jefferson et al. 2011 included four relevant case control studies involving Severe Acute Respiratory Syndrome or SARS and extent of gown wearing, all of which were conducted in hospitals. Evaluation against the AMSTAR II checklist, we judged the review to be of good quality. Univariate analysis indicated protection against infection from gown wearing (compared to not wearing) but in multivariate analysis the effect of gowns was not statistically significant. Gowns were generally worn as part of a larger bundle of PPE.
Simulated Exposure Studies
Verbeek et al. 2019 included 17 studies with 1950 participants evaluating 21 interventions. Evaluation against the AMSTAR II checklist, we judged the review to be of good quality. The review included 12 studies that simulated exposure either to droplets or splashed liquids. Of these, two studies Guo at al. 2014 (10) and Hall et al. 2018 (11) compared contamination relating to wearing and doffing of gown versus plastic apron. Both used a spray to simulate droplet spread. Guo compared disposable waterproof gown vs. apron; Hall compared ‘basic level’ personal protective equipment (PPE)– including mask, gloves, and apron– against various combinations of ‘suspected case’ PPE (all of which included respirator mask, gown or coverall, head covering, double gloves and boots) in a simulated exposure setting comparable to conducting AGPs. From the data in the original papers, it appears the aprons in Guo and Hall were both more substantial than those provided for frontline NHS staff.
Both studies found that wearing an apron led to more direct contamination from the spray and more indirect contamination and spillage during doffing compared to disposable waterproof gown (10). Hall at al. 2018 concluded that the ‘basic’ PPE described above was inadequate for high risk settings but insufficient data was provided to interpret that in the context of low-medium risk settings (11).
Observations of donning and doffing
Several studies have emphasised that while protective clothing and other measures provide protection during wear, donning and doffing PPE involves complex manoeuvres which are often unfamiliar to staff. Guideline violations and contamination are common, particularly during doffing. Practical training, rehearsal, and buddying all appear to improve protocol adherence.
Critical appraisal of the two systematic reviews
AMSTAR II checklist – Verbeek et al. 2019 and 2020:
- Did the research questions and inclusion criteria for the review include the components of PICO? Yes
- Did the report of the review contain an explicit statement that the review methods were established prior to conduct of the review and did the report justify any significant deviations from the protocol? Yes
- Did the review authors explain their selection of the study designs for inclusion in the review? Yes. Control studies.
- Did the authors use a comprehensive literature search strategy? Yes
- Did the authors perform study selection in duplicate? Yes
- Did the authors perform data extraction in duplicate? Yes
- Did the review authors provide a list of excluded studies and justify the exclusions? Yes
- Did the authors describe the included studies in adequate detail? Yes
- Did the review authors use a satisfactory technique for assessing the risk of bias (RoB) in individual studies that were included in the review? Yes
- Did the review authors report on the sources of funding for the studies included in the review? Yes
- If meta-analysis was justified did the review authors use appropriate methods for statistical combination of results? Yes
- If meta-analysis was performed did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis? Yes
- Did the review authors account for RoB in individual studies when interpreting/ discussing the results of the review? Yes
- Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? Yes
- If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? No – publication bias not discussed
- Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review? Yes
AMSTAR II checklist – Jefferson et al. 2011:
- Did the research questions and inclusion criteria for the review include the components of PICO? Yes
- Did the report of the review contain an explicit statement that the review methods were established prior to conduct of the review and did the report justify any significant deviations from the protocol? Yes
- Did the review authors explain their selection of the study designs for inclusion in the review? Yes. Comparative studies.
- Did the authors use a comprehensive literature search strategy? Yes
- Did the authors perform study selection in duplicate? Yes
- Did the authors perform data extraction in duplicate? Yes
- Did the review authors provide a list of excluded studies and justify the exclusions? No but justified exclusions
- Did the authors describe the included studies in adequate detail? Yes
- Did the review authors use a satisfactory technique for assessing RoB in individual studies that were included in the review? Yes
- Did the review authors report on the sources of funding for the studies included in the review? Yes
- If meta-analysis was justified did the review authors use appropriate methods for statistical combination of results? Yes
- If meta-analysis was performed did the review authors assess the potential impact of RoB in individual studies on the results of the meta-analysis or other evidence synthesis? Yes
- Did the review authors account for RoB in individual studies when interpreting/ discussin g the results of the review? Yes
- Did the review authors provide a satisfactory explanation for, and discussion of, any heterogeneity observed in the results of the review? Yes
- If they performed quantitative synthesis did the review authors carry out an adequate investigation of publication bias (small study bias) and discuss its likely impact on the results of the review? No – publication bias not discussed
- Did the review authors report any potential sources of conflict of interest, including any funding they received for conducting the review? Yes
REFERENCES
- The Lancet. COVID-19: protecting health-care workers. Lancet. 2020;395(10228):922.
- Chavez S, Long B, Koyfman A, Liang SY. Coronavirus Disease (COVID-19): A primer for emergency physicians. Am J Emerg Med. 2020.
- NHS England. Guidance and standard operating procedures: General practice in the context of coronavirus (COVID-19) Version 2.1. 2020. Accessed 9th April, 2020 at https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0133-COVID-19-Primary-Care-SOP-GP-practice_V2.1_6-April.pdf.
- World Health Organisation. Infection prevention and control during health care when COVID-19 is suspected: Interim guidance. Geneva: WHO; 19th March 2020. Accessed 6th April 2020 at https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125
- Centers for Disease Control and Prevention (US). Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. Atlanta: CDC; March 2020. Accessed 7th April 2020 at https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html.
- Verbeek JH, Rajamaki B, Ijaz S, Tikka C, Ruotsalainen JH, Edmond MB, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst Rev. 2019;7:CD011621.
- Jefferson T, Del Mar CB, Dooley L, Ferroni E, Al-Ansary LA, Bawazeer GA, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev. 2011(7):CD006207.
- Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database of Systematic Reviews. 2020(in press).
- French CE, McKenzie BC, Coope C, Rajanaidu S, Paranthaman K, Pebody R, et al. Risk of nosocomial respiratory syncytial virus infection and effectiveness of control measures to prevent transmission events: a systematic review. Influenza Other Respir Viruses. 2016;10(4):268-90.
- Guo YP, Li Y, Wong PL. Environment and body contamination: a comparison of two different removal methods in three types of personal protective clothing. Am J Infect Control. 2014;42(4):e39-45.
- Hall S, Poller B, Bailey C, Gregory S, Clark R, Roberts P, et al. Use of ultraviolet-fluorescence-based simulation in evaluation of personal protective equipment worn for first assessment and care of a patient with suspected high-consequence infectious disease. J Hosp Infect. 2018;99(2):218-28.

