Spreading SARS-CoV-2 through ocular fluids
March 20, 2020
Spreading SARS-CoV-2 through ocular fluids PDF to download
Robin E Ferner, Philip I Murray, Professor of Ophthalmology, University of Birmingham, UK and Jeffrey K Aronson
On behalf of the Oxford COVID-19 Evidence Service Team
Centre for Evidence-Based Medicine, Nuffield Department of Primary Care Health Sciences
University of Oxford
Correspondence to cebm@phc.ox.ac.uk
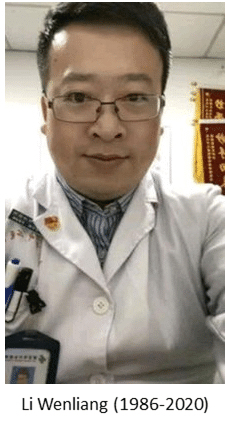 The death of the Chinese ophthalmologist Li Wenliang in Wuhan last month raised many concerns. Here we examine one of them: the possibility that the β-coronavirus that causes COVID-19, SARS-CoV-2 (also called 2019-nCoV) can affect the eyes, causing conjunctivitis and—perhaps whether there is conjunctivitis or not—having the potential to transmit the virus via ocular fluids.
The death of the Chinese ophthalmologist Li Wenliang in Wuhan last month raised many concerns. Here we examine one of them: the possibility that the β-coronavirus that causes COVID-19, SARS-CoV-2 (also called 2019-nCoV) can affect the eyes, causing conjunctivitis and—perhaps whether there is conjunctivitis or not—having the potential to transmit the virus via ocular fluids.
SARS-COV-2 is an encapsulated single-stranded RNA virus that has a spike glycoprotein, which interacts with a receptor-binding domain. The receptor is angiotensin-converting enzyme 2 (ACE-2), which is expressed in the membranes of many cells in the body, including the respiratory, renal, and intestinal tracts, and on cardiac and immune cells. SARS-CoV-2 has been detected in blood, sputum, urine, faeces, and respiratory secretions from infected patients. ACE-2 has been demonstrated in aqueous humour and retina, but not on conjunctival or corneal epithelia.
Coronavirus, bound to its receptor on the cell surface, is internalized by endocytosis, replicates, and is released to infect further cells. Infection can lead to cytokine dysregulation, which is responsible for the potentially fatal acute respiratory illness.
Viruses that cause respiratory illnesses can also cause ocular complications in infected individuals and can establish respiratory infections after ocular exposure. For example, in ferrets aerosols of influenza viruses can mediate respiratory transmission of the virus to healthy animals.
Some coronaviruses are reported to cause conjunctivitis in humans. However, the receptor-binding domain is not the same for all coronaviruses, so this provides insufficient evidence to demonstrate that SARS-CoV-2 will be transmissible through the conjunctiva. SARS-CoV-1 (formerly SARS-CoV) does bind to ACE-2, and appears to infect similar cell lines in vitro. Since ACE-2 receptors have not been demonstrated in the conjunctiva or cornea, transmission from droplet spread may occur when viral particles in tears are drained through the nasolacrimal duct into the respiratory tract.
SARS-CoV-1
SARS-CoV-1 virus was not detected by reverse transcriptase polymerase chain reaction (RT-PCR) or isolated by viral culture from tears or conjunctival scrapings obtained from 20 patients with SARS-CoV-1 infection during the Hong Kong outbreak in 2003. On the other hand, tear samples were positive for viral RNA during the first nine days of their illness in three of 36 patients with SARS-CoV-1 infection in Singapore.
SARS-CoV-2
A study of conjunctival swabs from patients with COVID-19 but without ocular symptoms yielded one clear positive result for viral RNA, and two probably positive results. In 31 patients with SARS-CoV-2 infection, nine of whom were severely affected, samples of tears and conjunctival secretions gave positive results by RT-PCR in only one patient, who had conjunctivitis.
There have also been anecdotal reports of a doctor who had cared for patients with COVID-19, and who developed conjunctivitis “several days before the onset of pneumonia,” and a Chinese patient in France who presented with fever, rigors, fatigue, conjunctivitis, and cough. The WHO-China Joint Mission on COVID-19 estimated the incidence of conjunctival congestion at 0.8%, based on a study in 55,924 laboratory-confirmed cases.
Other coronaviruses
HCoV-NL63, the New Haven coronavirus, was first identified in a baby with bronchiolitis and conjunctivitis and later in three children with conjunctivitis associated with HCoV-NL63 respiratory tract infections. However, clinical reports suggest a low incidence of conjunctivitis with other coronaviruses. For example, it was recorded in 6 of 261 cases of infection (2%) with Middle East respiratory syndrome coronavirus (MERS-CoV). Conjunctival swabs from 5/76 Omani dromedary camels (7%), the animal host, proved positive for viral RNA.
Advice to ophthalmologists
The close proximity between ophthalmologists and their patients has raised concerns because they are at risk of infection through transmission by droplets from coughs or sneezes. For asymptomatic patients with no risk factors, the American Academy of Ophthalmologists (AAO) and the UK’s Royal College of Ophthalmologists (RCOphth) recommend generic measures to protect ophthalmologists from infection, and these include scrupulous disinfection practices, protective plastic slit-lamp breath shields, reducing or eliminating conversations with the patient during slit-lamp examination, limiting the time spent with the patient at the slit lamp¸ and considering whether ophthalmic investigations, such as ocular imaging, are critical to the decision-making process. Both organizations have recommended that non-urgent treatments be cancelled.
Conclusions
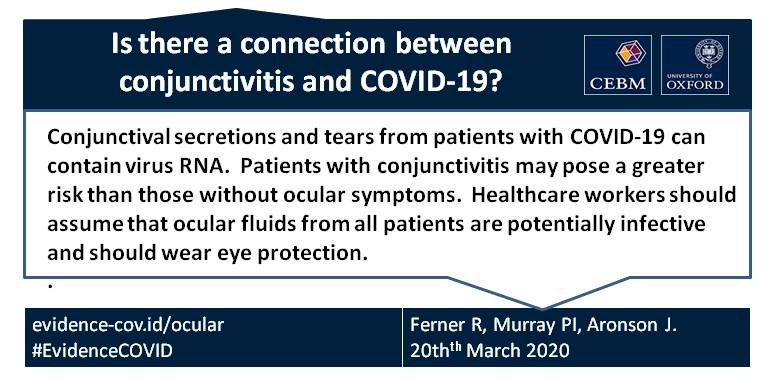
- The evidence so far is that conjunctival secretions and tears from patients with SARS-CoV-2 infection can contain virus RNA.
- Under 1% of patients with the infection will have conjunctivitis. They may pose a greater risk than those without ocular symptoms.
- Healthcare workers should assume that ocular fluids from all patients are potentially infective.
- Healthcare workers should wear eye protection when dealing with patients who have or may have COVID-19.
Disclaimer: the article has not been peer-reviewed and the sources cited should be checked. The views expressed in this commentary represent the views of the authors and not necessarily those of the host institution, the NHS, the NIHR, or the Department of Health and Social Care. The views are not a substitute for professional medical advice.
We welcome feedback on this page and if there are errors or omissions then please let us know at cebm@phc.ox.ac.uk

