What is the efficacy and safety of rapid exercise tests for exertional desaturation in covid-19?
April 21, 2020
Trisha Greenhalgh
Babak Javid [1]
Matthew Knight [2]
Matt Inada-Kim [3]
With search input from Jon Brassey and Helen Williams
(see ‘search strategy’ below)
On behalf of the Oxford COVID-19 Evidence Service Team
Centre for Evidence-Based Medicine, Nuffield Department of Primary Care Health Sciences
University of Oxford
[1] Tsinghua University School of Medicine, Beijing, CHINA 100084
[2] West Hertfordshire Hospitals NHS Trust
[3] Hampshire Hospitals NHS Foundation Trust
Correspondence to trish.greenhalgh@phc.px.ac.uk
VERDICT
Two tests have potential: the 1-minute sit-to-stand test (in which the patient goes from sit to stand as many times as they can in one minute) and the 40-step test (in which the patient takes 40 steps on a flat surface). The former correlates well with the validated 6-minute exercise test. The latter is less demanding (hence safer) and in more widespread use, but does not appear to have been validated. There is no evidence of harm (e.g. precipitation of cardiopulmonary compromise) from either test, but neither is there firm confirmation of their safety. Neither test has been studied in the context of covid-19; they were validated on patients with chronic interstitial lung disease and airways obstruction. An exertional desaturation test should be used with clinical judgement, and only on patients whose resting oximetry reading is 96% or above unless they are in a supervised care setting. It should be terminated if the patient experiences adverse effects.
BACKGROUND
The assessment of the breathless or unwell patient with symptoms of covid-19 should include oximetry.1 Furthermore, it is becoming clear that some patients have normal pulse oximetry at rest but their readings deteriorate on exertion (unpublished data). Indeed, front-line clinicians have identified the late transfer of patients with exertional desaturation (i.e. a fall of 3% or more in pulse oximetry reading on exercise) as a possibly remediable cause of poor outcome. In other words, if we could better identify those with exertional desaturation and escalate their care more promptly, we could reduce mortality. The question then becomes: which test should we use to confirm or exclude exertional desaturation?
This question needs to be answered in the context of current care arrangements, in which most patients are initially assessed remotely (by phone or video). Oximeters in smartphone apps are unreliable, so an approved and tested medical-grade oximeter should be supplied to the patient. This is happening in some localities as part of ‘virtual ward’ arrangements.
OVERVIEW OF EXERTIONAL TESTS
Tests of exertion in lung disease have mostly addressed the monitoring over time of chronic lung disease and have been oriented to measuring exercise capacity. A helpful narrative review by Lee et al (which drew on an earlier systematic review by European Respiratory Society and American Thoracic Society2) lists, for example, a 30-minute walk test, a 4-minute walk test, a stair climb power test (10 flights), a more moderate stair climb test (un-standardised but based on the patient’s own home stairs), 6-minute and 3-minute step tests, a 15-step test (step up and down on a 25 cm platform 15 times as fast as possible), Chester step test (an incremental protocol on a 20 cm platform with 2-minute phases commencing with 15 steps per minute and increasing by 2 per minute till terminated by dyspnoea or fatigue), and modified Chester step test (starting at 10 steps per minute).3 These authors also describe three different sit-to-stand tests: five repetition sit-to-stand (5-min STS: patient stands up fully and sits down 5 times as quickly as they can); 1-minute sit to stand test (1-min STS: patient stands up fully and sits down as many times as they can in one minute) and the 30-second and 2-minute variants of this.3 They also review tasks based on activities of daily living such as a semi-standardised “grocery shelving task”.3
All the exercises described by Lee et al in the above review were designed mainly for longitudinal monitoring of the severity of chronic lung disease, and several have been shown to correlate with survival. The tests combine an assessment of lung function with that of general physical fitness and muscle strength – a useful composite measure in patients with (for example) chronic obstructive pulmonary disease. They were not originally designed with assessment of acute breathlessness in mind, but as described below, some have subsequently been evaluated for that purpose.
A recent systematic review considered the validity of the 1-minute sit-to-stand test in measuring exercise capacity in patients with chronic lung disease.4 The main focus of this review was on a) whether the test correlated with severity of lung disease (broadly, it did), the test-retest reliability of the test (it appeared to be high), and whether the test score correlates with the gold standard 6-minute walk test (it did). They concluded that “The 1-MSTST appears to be a practical, reliable, valid, and responsive alternative for measuring exercise capacity, particularly where space and time are limited.”4 However, these authors did not look at the 1-minute sit-to-stand test in the assessment of exertional desaturation.
Fox et al have explored the use of oximetry along with step climbing tests in the detailed assessment of pulmonary capacity, using area under the curve of a continuous oximetry reading.5 Whilst these authors found that oximetry thus measured correlated with severity of disease and survival, such an approach is not relevant to the remote assessment of the acutely breathless or hypoxic patient. Similarly, a study of oximetry in the 6-minute walk test showed strong correlation with disease severity and survival,6 but the test does not transfer to the current covid-19 situation.
EXERTIONAL TESTS FOR MEASURING DESATURATION IN COVID-19
We found no published literature describing validation of exertional desaturation tests in covid-19.
EXERTIONAL TESTS FOR MEASURING DESATURATION IN OTHER CONDITIONS
Briand et al, in a clinic population of 107 patients with chronic interstitial lung disease, compared the nadir SpO2 measured by oximetry on the 6-minute walk test (6MWT) and the 1-minute sit-to-stand (1MSTS) test, performed on the same day.7 There was high correlation between these (r = 0.9; p < 0.0001; Figure 1).
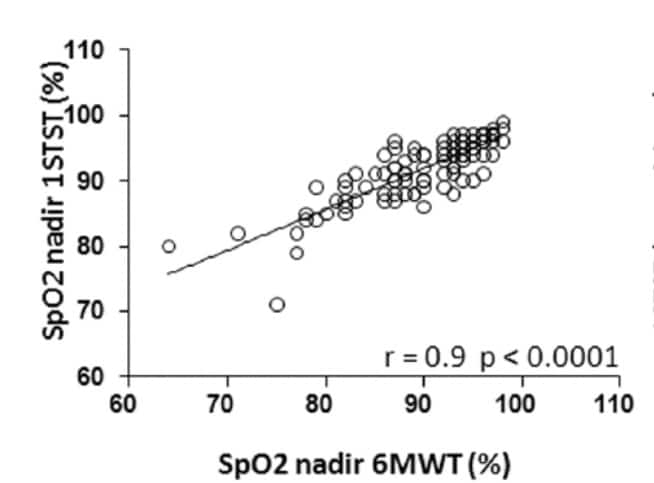
Figure 1 (reproduced from Briand et al7) showing correlation in patients with chronic lung disease between 6-minute walk test and 1-minute sit-to-stand test in nadir of SpO2
Briand et al also found that the correlation between the tests in terms of desaturation appeared to hold at lower levels of SpO2 (Figure 2). The authors commented:
“The 6MWT and 1STST showed good agreement in their ability to detect oxygen desaturation ⩾4%, with a κ coefficient of 0.68 (95% CI 0.54–0.82). The number of patients showing desaturation levels ⩾4% during only one of the two tests was not significantly different between the 1STST (n=11) and the 6MWT (n=6). Strong correlations were found between the SpO2 nadir during the 1STST and 6MWT (r = 0.76, p < 0.0001) for patients with oxygen desaturation below 88% during the 6MWT.”
No adverse events were described in this study.
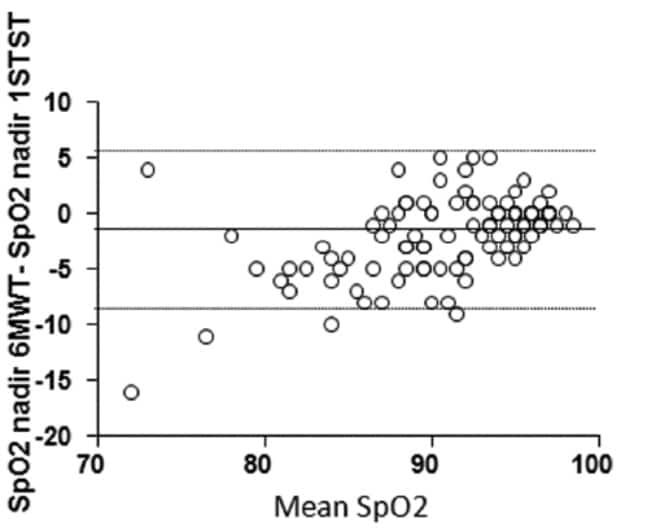
Figure 2 (reproduced from Briand et al7) showing Bland-Altman plot of difference in SpO2 nadir between 6-minute walk test and 1-minute sit-to-stand test as a function of mean SpO2 nadir in both tests (horizontal lines show mean difference and 95% Cis)
In another (much smaller) study, on a sample of patients with chronic obstructive lung disease, Crook et al compared the 1-minute sit-to-stand test with 5 sit-to-stand test (in which the patient did 5 repeats of sit-to-stand), and the 6-minute walk test, in three situations: resting, nadir during exercise, and recovery.8 Their findings are summarised in Table 1
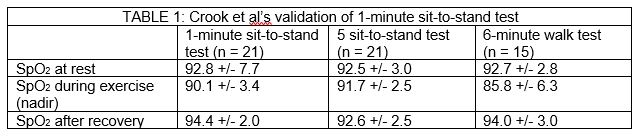
The authors commented: “When using the lowest SpO2 value in the first minute after exercise, desaturation was detected in four additional patients for the 1-min STS test.”
The Crook study was probably underpowered to demonstrate a statistically significant difference between the 6MWT (undertaken on only 15 patients) and the 1MSTS, but it is likely that a larger study would have shown the latter (a less physically demanding test) to be less sensitive to desaturation. However, the 1MSTS patients did show desaturations up to one minute after stopping the test, so patients need to be advised to monitor their saturations for at least this long after the exercise period. Indeed, analysis of individual data reveals that all patients who showed desaturation in the 6MWT also showed desaturation in the 1MSTS test if extended to a full minute post recovery.
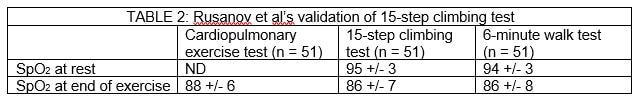
Rusanov et al validated the 15-step climbing test against the 6-minute walk test in 51 patients with pulmonary fibrosis.9 Their findings, shown in Table 2, confirm the high correlation between the two tests. Another paper by the same authors reports duplicate findings.10
Another study found high correlation between desaturation levels on the 6-minute walk test and a shorter 2-minute walk test in a small sample of 26 patients with COPD.11
The test that is most used in acute practice is the 40-step walk test – the patient is asked to walk 40 steps on the flat and oximetry repeated. We found no research studies on this at all.
All the above studies were undertaken in patients with airways obstruction (e.g. COPD) or interstitial lung disease (most commonly idiopathic pulmonary fibrosis). These are diseases of ventilation. Patients with covid-19 may have normal ventilation but significant problems with oxygen diffusion (because the underlying pathology is more of an inflammatory pneumonitis than a true pneumonia).12 In that sense, covid-19 seems to behave more like pneumocystis carinii pneumonia (PCP) – another acute infectious lung disease which presents with dry cough, silent hypoxia, exertional desaturation and similar CT scan changes.13
In a small study from 1988 of 39 patients with PCP (all HIV-positive young men), exertional desaturation was demonstrated in most of them (including many who had normal saturation at rest) using a 10-minute cycling test, whereas patients who presented with other acute lung conditions including bacterial pneumonia, tuberculosis and pulmonary candidiasis did not show exertional desatruation.13
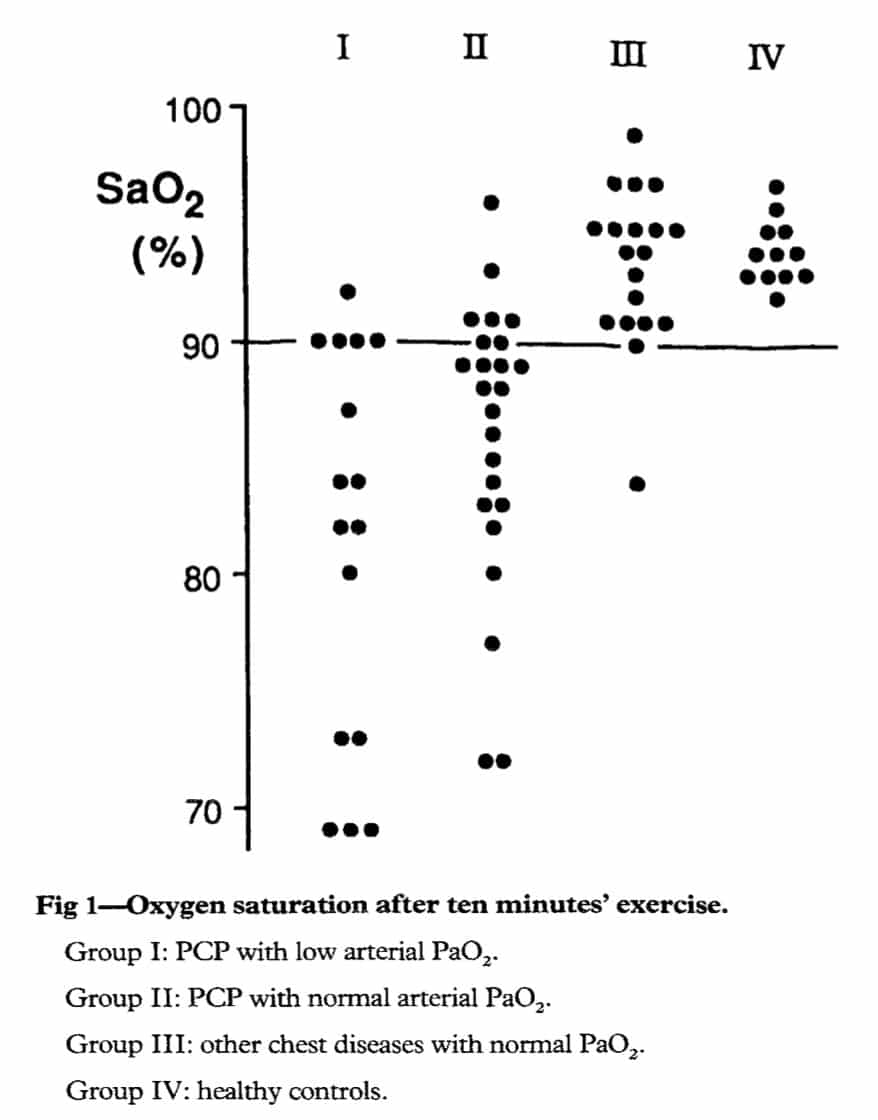
Figure 3 (reproduced from Smith et al13) showing exertional desaturation (after ten minutes’ cycling) in those with pneumocystis carinii pneumonia (groups I and II) but not those with other lung disease (group III) or healthy controls (group IV)
CLINICAL COMMENTARY
The clinical similarities between covid-19 pneumonia and PCP (likely, both diseases of perfusion not ventilation) supports a conservative and risk adverse approach to aggressive exercise testing in the home environment. The desaturation observed in the patients with chronic lung disease in the brief exercise tests7 8 are likely to be more marked in those with covid-19. For this reason, even a small desaturation on exercise should alert the clinician and a drop of 3% should be cause for serious concern, regardless of the amount of exercise needed to produce it.
The ’40 steps around the room test’ (in a patient able to stand safely unaided and whose resting saturation is 96% or above) is the lowest level of exertion of any test either in the literature or in clinical practice. This is appropriate given the high-risk group and the home environment (no clinician on hand to guide or resuscitate). This test will likely have a low sensitivity but if positive will be highly specific and warrant urgent assessment.
If the 1MSTS is used, it should be followed by monitoring for at least one minute to observe for desaturation.
Risk to the patient from exercise tests should be considered. Patients should be advised to terminate promptly if they develop any adverse symptoms (severe breathlessness, chest pain, dizziness). Tests involving climbing a flight of stairs should be avoided since the stairs is a dangerous place to collapse. A formal 6MWT is not necessary in the home environment but may be useful in following up patients in a clinic or inpatient setting. When doing these more strenuous exertion tests, carefully observe the patient and also make a clinical judgement based on severe fatigue and tachypnoea.
CONCLUSIONS
Covid-19 may cause an unusual form of acute lung disease characterised by a tendency to desaturate on minimal exertion. The 40-step test (which is in widespread clinical use but has not been validated) and the 1-minute sit-to-stand test are the least demanding tests and therefore the most appropriate for recommending to patients at home. They are likely to be specific but not sensitive (that is, a positive test is serious cause for concern but a negative test should not necessarily reassure).
More research is needed on exertional desaturation tests in all settings (GP, emergency department, ambulance), in the context of covid-19.
Disclaimer: the article has not been peer-reviewed; it should not replace individual clinical judgement and the sources cited should be checked. The views expressed in this commentary represent the views of the authors and not necessarily those of the host institution, the NHS, the NIHR, or the Department of Health and Social Care. The views are not a substitute for professional medical advice.
SEARCH STRATEGY
Two independent searches were done – one by Jon Brassey of Trip, and one by Helen Williams of Hampshire Healthcare Library Service.
Databases searched by JB were LitCovid, Scholar and Google. The terms were:
- step test or field test
- hypoxia or exertional desaturation
From these, promising articles were then used to find additional documents via two methods:
- Forward and backward citation matching
- Related articles (also used Microsoft Academic Search for this)
Databases searched by HW were AMED, CINAHL, EMBASE MEDLINE, and PubMedusing the over-arching question ‘Very short exercise desaturation tests for use in ED’. Search terms were:
- (quick OR short) AND oxygen) AND exercise) AND (desaturation OR saturation)) AND test*(“emergency department*” AND oxygen) AND exercise) AND desaturation) AND test*)
- (“emergency department*” AND oxygen) AND exercise) AND saturation) AND test*)
- (“emergency department*” AND oxygen) AND exercise) AND desaturation)
- (“emergency department*” AND oxygen) AND exercise) AND saturation)
- (1-min sit-to-stand test) or (“1 min sit to stand test”) or (“one minute sit to stand”)
REFERENCES
- National Institute for Health and Clincial Excellence. COVID-19 rapid guideline: managing suspected or confirmed pneumonia in adults in the community. London: NICE 2020. Accessed 4th April 2020 at https://www.nice.org.uk/guidance/ng165.
- Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease: Eur Respiratory Soc, 2014.
- Lee A, Harrison S, Beauchamp MK, et al. Alternative field exercise tests for people with respiratory conditions. Current Physical Medicine and Rehabilitation Reports 2015;3(3):232-41.
- Bohannon RW, Crouch R. 1-Minute Sit-to-Stand Test: Systematic Review of Procedures, Performance, and Clinimetric Properties. Journal of cardiopulmonary rehabilitation and prevention 2019;39(1):2-8.
- Fox BD, Sheffy N, Vainshelboim B, et al. Step oximetry test: a validation study. BMJ open respiratory research 2018;5(1):e000320.
- Lancaster LH. Utility of the six-minute walk test in patients with idiopathic pulmonary fibrosis. Multidisciplinary respiratory medicine 2018;13(1):1-7.
- Briand J, Behal H, Chenivesse C, et al. The 1-minute sit-to-stand test to detect exercise-induced oxygen desaturation in patients with interstitial lung disease. Therapeutic advances in respiratory disease 2018;12:1753466618793028.
- Crook S, Büsching G, Schultz K, et al. A multicentre validation of the 1-min sit-to-stand test in patients with COPD. European Respiratory Journal 2017;49(3):1601871.
- Rusanov V, Shitrit D, Fox B, et al. Use of the 15-steps climbing exercise oximetry test in patients with idiopathic pulmonary fibrosis. Respiratory medicine 2008;102(7):1080-88.
- Shitrit D, Rusanov V, Peled N, et al. The 15-step oximetry test: a reliable tool to identify candidates for lung transplantation among patients with idiopathic pulmonary fibrosis. The Journal of heart and lung transplantation 2009;28(4):328-33.
- Gloeckl R, Teschler S, Jarosch I, et al. Comparison of two-and six-minute walk tests in detecting oxygen desaturation in patients with severe chronic obstructive pulmonary disease—A randomized crossover trial. Chronic respiratory disease 2016;13(3):256-63.
- Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Medicine 2020:1.
- Smith D, Wyatt J, McLuckie A, et al. Severe exercise hypoxaemia with normal or near normal X-rays: a feature of Pneumocystis carinii infection. The Lancet 1988;332(8619):1049-51.

